January is National Poverty in America Awareness Month, an observance with roots dating back to the 1960s. This month-long observance was created to bring awareness to the unique challenges faced by those who qualify as “poor” in the United States (US). In 2023, over 11% of the US population lived in poverty, equating to almost 40M people. Not having enough money for essentials often leads to serious issues like food insecurity, homelessness, and the inability to afford basic necessities.
Poverty has traditionally been a leading socioeconomic barrier to healthcare access and clinical trial participation. A study on cancer trial participation determined that patients with annual household incomes less than $50K were 27% less likely to participate in a clinical trial. This vulnerable population requires specialized support services to increase access to medical care and research options. Individuals living below the poverty level have worse health outcomes and lower life expectancies due to limited healthcare and other resources. One study compared the top and bottom 1% of income and found a 10 -14-year life expectancy disparity between the two groups.
What Qualifies as “Poverty” in America?
The US Department of Health and Human Services (HHS) is the federal agency that determines the Federal Poverty Level (FPL) guidelines. These guidelines are revised annually and result from the Poverty Thresholds set by another government agency, the US Census Bureau. Additional clarification on the two agencies and their functions related to poverty can be found here.
Two primary metrics are factored in when defining FPL: yearly income level and household size. In 2024, poverty levels for the 48 contiguous states and the District of Columbia are as follows:
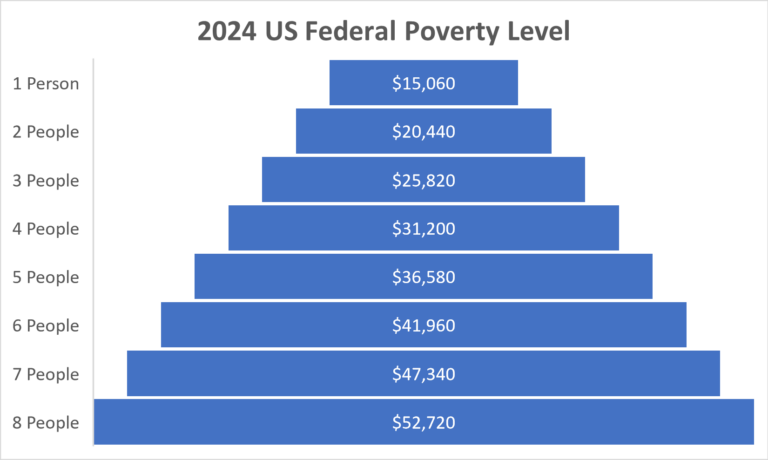
For households with more than 8 people, $5,380 per person is added to the above totals.
In Alaska and Hawaii, these guidelines levels are a bit higher, as the cost of living is higher in these two states:
- Alaska: $18,810 – $65,920 for 1-8 people; $6,730 per person for additional people
- Hawaii: $17,310 – $60,640 for 1-8 people; $6,190 per person for additional people
Additional Layer of Financial Challenges for Those with a Serious Illness
Families falling under the FPL who are dealing with a chronic or rare disease often have increased financial burdens to consider. They may have more people living in the home to provide care for the ill patient, and the level of care needed can prevent adults from outside employment opportunities with much-needed salary and insurance benefits. This socioeconomic group often feels hopeless and stuck in an inescapable cycle of poverty. Due to issues like low education levels and limited access to healthcare options, members of this group may never learn of new treatment options via a clinical study. Conversely, they may know of an opportunity, but the emotional, financial, and logistical barriers to trial participation are too burdensome to justify participation.
US Government Assistance Programs to Support the Poor
The annual FPL amounts shown above are used to establish financial eligibility for various federally funded low or no-cost public assistance programs, such as Medicaid and Medicare, both instituted by the US Government in the mid-1960s to assist specific at-risk populations in the US:
- Medicaid: Medicaid is a federal healthcare insurance program to assist low-income and elderly adults, pregnant women, children, and those with disabilities. Individual states within the US administer the Medicaid program, so coverage often varies between states. Currently, over 81M people in the US receive Medicaid coverage. Medicaid receives funding from the US federal government and individual state governments. Recent reports estimate the government is responsible for 64% of total Medicaid costs, with state governments contributing 36%.
- Medicare: Medicare is a federal healthcare insurance program to assist specific demographic groups within the US, including those 65 and older and younger individuals with disabilities or severe chronic diseases. Currently, over 65M people in the US receive Medicare coverage. Medicare is a federally funded program, primarily backed by the US Social Security Administration (SSA) and supported by US taxpayers. Currently, 1.45% of all earnings are taken from employee paychecks for the Federal Insurance Contributions Act (FICA), and employers match another 1.45%, bringing the total to a 2.9% contribution to Medicare.
- Social Security: In the 1930s, the US Government enacted the Social Security Act to provide income to senior citizens upon their retirement from the US workforce. Monies for this service come through the FICA Act cited above, and the amount one can collect monthly is based upon an individual’s lifetime earnings. Full benefits can be collected at the age of 67, with reduced benefit eligibility at the age of 62.
- Welfare: Also in the 1930s, the US Government began to create the programs now known collectively as the Welfare System. Today, the program comprises 14 programs overseen by eight separate federal agencies. Eligibility for each of the programs is based on financial need, with amounts adjusted yearly based on cost-of-living considerations.
Retaining Eligibility in Government Programs While Participating in Clinical Trials
Participants in clinical research often receive financial reimbursement for attending their clinical site visits and for incidental expenses incurred due to the travel involved in participation. Individuals enrolled in the above programs are often hesitant to participate in clinical studies because of the possibility that the payments they receive over the term of the trial could negatively impact their welfare eligibility status. Clinical trials that partner with a patient concierge services company provide the participant with a single point of contact who is knowledgeable about the trial reimbursement process and can help them navigate any potential questions or concerns.
Poverty as a Barrier to Clinical Trial Participation
Access to and diversity within clinical research has historically been a significant issue within the clinical trial industry. Those with a higher socioeconomic status can more often participate in clinical trials, as they can better navigate the added expenses related to trial participation, such as:
- Out-of-Pocket Expenses: Individuals struggling with poverty often do not have much, if any, disposable income remaining after meeting their monthly necessities, making participation in a trial seem out of reach. In general, paying for parking at a medical center or a meal during a long day at a clinical site would not be a financial stretch. For people with low incomes, however, these added costs deter many from receiving much-needed treatment. In one case, a participant reported packing a lunch to take along because they could not afford the cost of eating out.
- Accommodation: Many individuals facing poverty have no disposable income available to secure additional housing options during the clinical site visits often required with participation in a research study. One participant reported:
“I had to find a homeless shelter to stay in after the study. It wasn't in any condition to cater to someone who just had a stem cell transplant. I had to get my family from out of state to come get me as I was in no condition to drive or fly.”

- Time Away From Work: It can be assumed that many employed yet poor hold hourly or minimum-wage jobs, offering very little or no paid time off. For those with these types of jobs, not showing up for work equates to not getting paid. For someone struggling with a chronic or rare disease, missing work may happen often due to the illness and can result in the loss of their job. It is extremely difficult for these individuals to consider clinical trial participation, which would result in additional time away from work. The stress is felt equally by those who function as a caregiver for someone in a clinical trial. One participant reported:

“Financial issues are definitely the hardest thing - it's really good when they reimburse you for your time. The family having to take that time off has been the hardest thing to coordinate.”
Clincierge conducted a two-phase Voice of the Patient research study to understand better the emotional, financial, and logistic burdens of clinical trial participation. The study found patients and caregivers alike were worried about taking time off work and reported missed site visits due to work responsibilities.
- 47% of patients and 65% of caregivers worried about taking time off work for trial visits
- 29% of patients and 17% of caregivers reported missing study visits because of work restrictions
- Rural Populations: At times, location can be a contributor to poverty and seen as a barrier to trial enrollment, especially in rural or remote areas of the world. In parts of Latin America and the United Kingdom, for example, the following issues have been reported as challenges:
- Lower education levels, higher rates of illiteracy
- Language challenges, unique dialects spoken in rural communities
- Lack of access to technology and the Internet
- Never exposed to travel, don’t know what to expect or how to plan
- Living too far away from medical centers, “off-the-grid”
- Closest medical facility can be across a country border, posing unique challenges
There are many underlying issues to the whole of poverty, and much work must be done moving forward to increase access to clinical trials for those identifying with this socioeconomic subgroup.
Using a Patient Concierge Services Provider to Increase Access to Clinical Trials
Clinical trial sponsors and clinical research organizations (CROs) looking to increase access and diversity in their studies first need to consider the individual needs of the patient and their barriers to clinical trial participation. Whether these challenges are perceived or actual, they often deter participants from enrolling in a trial. For those with a chronic or rare disease, this study may be their only option for a potentially life-changing treatment.
One of the main barriers to study enrollment and retention for those facing poverty is the inability to pay for additional expenses incurred throughout the trial. When study sponsors and CROs partner with a patient concierge services company that will pre-plan and prepay for hotel accommodations, ground transportation, flight and rail ticketing, and assist with reimbursements and stipend payments, the stress of being “too poor” to participate is removed. With this financial strain eased, the patient can better focus on the treatment provided, while caregivers can tend to the patient’s needs. This partnership shows a commitment to the individual patient and caregiver and the overarching goal of achieving healthcare equity and inclusion.

Additional Resources:
Learn how patient concierge services remove barriers to trial participation in our blog, Caring for Rare: The Elevated Cost of Rare Disease Patient Care.
- Patients, Poverty, and Participation in Research: The Hidden Costs of Disease and Socioeconomic Status
- 2023 Poverty Levels/Guidelines & How They Determine Medicaid Eligibility
- January is National Poverty in America Awareness Month
#NationalPovertyinAmericaAwarenessMonth #povertyawareness #accessanddiversity #eradicatepoverty #dei


