A recent study by the National Institute of Health’s National Center for Advancing Translational Sciences (NCATS) found the costs associated with rare disease patient care are between three to five times higher than the costs to treat those with more common illnesses.
In the United States, a rare disease affects less than 1 in 200,000 people. Currently, over 7,000 rare diseases have been identified, with less than 10% of these having a treatment approved by the US Food and Drug Administration (FDA). Rare diseases collectively affect 25 to 30 million Americans and are often genetic in nature, thus affecting children and adolescents in disproportionate numbers.
An article published in the October 2021 issue of the Orphanet Journal of Rare Diseases references the NCATS study and cites the potential effects on various healthcare industry sectors.
The pilot study reviewed patient records and billing codes to determine if the individual had received a rare disease diagnosis. They identified 14 rare diseases and focused on the cost of the treatment for these patients versus the cost of treatment for patients with a common disease diagnosis. The diseases chosen were diverse, including various age groups, affected organ systems, and disease severities.
The study found the rare disease cost per patient per year exceeded the non-rare cost per patient per year in every case analyzed. Rare disease patients often receive a diagnosis at a younger age and their conditions are usually more severe. They require more time in doctors’ offices and hospitals over their lifetime, resulting in larger medical bills.
As a result, the study’s final analysis reported that treatment of the 25 to 30 million rare disease patients in the United States results in an annual medical expenditure of $400 billion. This amount equates to the total annual medical costs of treating Americans with more common diseases like Alzheimer’s disease, cancer, and heart failure.
Below we look at several categories within the United States healthcare system and how these findings affect each one:
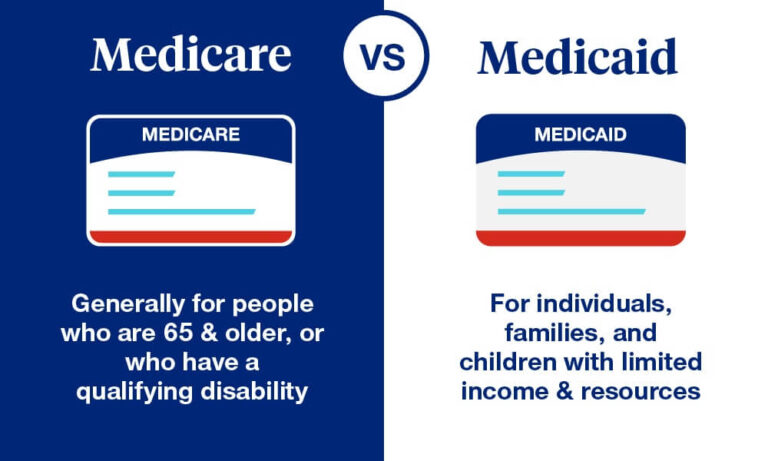
Medicare
- Medicare is a federal healthcare insurance program to assist specific groups within the United States, including those 65 and older and younger individuals with disabilities or severe chronic diseases like kidney failure. Medicare is a federally funded program.
Medicaid
- Medicaid is a federal healthcare insurance program to assist low-income and elderly adults, pregnant women, children, and those with disabilities. Individual states within the United States administer the Medicaid program, so coverage often varies. The funding for Medicaid comes from both the federal government and the individual states.
Medicare is funded primarily by the United States Social Security Administration, which in turn is supported by United States taxpayers. Currently, 1.45% of all earnings are taken from paychecks for the Federal Insurance Contributions Act (FICA), and employers match another 1.45%, bringing the total to a 2.9% contribution.
Alternatively, Medicaid receives funding from the US federal government and individual state governments. Recent reports estimate the government pays 64% of total Medicaid costs, with state governments contributing 36%.
Subsequently, the elevated cost of treating rare disease patients could translate into the need for additional funding for both Medicare and Medicaid. This increase could result in higher FICA taxes for individuals and their employers and higher contributions required from the federal and state governments.
Healthcare Industry
- The Kaiser Family Foundation recently reported that about half of US residents receive their health insurance through their employer. Known as group health insurance, employees can often choose between several plan options with tiered pricing. If an individual’s employer does not offer group healthcare insurance or a person is unemployed, there are several options to self-purchase healthcare coverage. However, this option can require specific medical tests and a physical examination before acceptance, and it is often more expensive than other options.
Employees generally share the cost of healthcare coverage with their employers, with many deducting a monthly fee for coverage directly from their paycheck, while others choose free or low-cost programs with higher costs for visits to the doctors, hospitalizations, and medications.
Again, as costs for rare disease patient treatments continue to rise, costs to employers and employees alike may need to increase as well.
On average, it takes seven years for a patient to receive a rare disease diagnosis. These years are often filled with many diagnostic tests, visits to various doctors and hospitals, and a sense of uncertainty and fear. As we are learning from rare disease patients, the diagnosis itself is just the beginning of a much longer treatment journey, if one even exists.
In a Voice of the Patient research study recently conducted by Clincierge, rare disease patients shared the many barriers to clinical trial participation. After reviewing participants’ responses, the complexity of navigating the health insurance process was a commonly cited barrier.
When asked about the most challenging part of clinical trial participation, one patient responded,
"For me, it was the relocation issues of setting up in another state and the health insurance changes to get the care and medications I needed not related directly to the trial. I went from a state with a generous Medicaid program to a much less generous state. And I was just there for a short time so going through the process was difficult to find the funding for what I needed. I have a lot of experience with these issues, so I managed to work through it, but it was difficult and may be overwhelming for other families."
In short, it is clear rare disease patients and their caregivers would benefit significantly from educational resources and guidance from their insurance providers to assist them in understanding treatment options like clinical trial participation. The patient concierge coordinators of Clincierge are paired one-on-one with rare disease trial participants and their caregivers to support them throughout the clinical trial. When clinical trial stakeholders collaborate and offer resources to remove the many emotional, financial, and logistical burdens these patients face, it significantly increases the ability for participants to enroll in new treatment options and continue in the study through trial completion.